Introduction of preventive vaccines
A vaccine is essentially a treatment that generates an immune response and helps combat various diseases by providing protection to patient specific cells by activating T cells and B cells to help fight off the disease and provide protection to the body. Vaccines can help protect against certain diseases by imitating an infection. This type of imitation infection helps teach the immune system how to fight off a future infection. Sometimes, after getting a vaccine, the imitation infection can cause the body temperature to rise in order to initiate the immune buildup response. Once the vaccinated body has an adequate supply of T-lymphocytes and B-lymphocytes, it will create an immune memory of how to combat certain foreign cells. However, it typically takes a few weeks for the body to produce T-lymphocytes and B-lymphocytes after vaccination. Therefore, it is possible that a person infected with a disease just before or just after vaccination could develop symptoms and get that disease, because the vaccine has not had enough time to provide protection. While vaccines are the safest way to protect a person from a disease, no vaccine is perfect. It is possible to get a disease even when vaccinated, but the person is less likely to become seriously ill.
(Sources: Centers for Disease Control and The University of Chicago Medical Center)
Brief history of preventive vaccines
The first disease eradicated by a vaccine was smallpox in 1798. This vaccine was invented by the brilliant British physician and scientist, Edward Jenner. The term vaccine and vaccination are derived from Variolae vaccinae (smallpox of the cow), which was devised by Jenner to denote cowpox. He used the phrase in his research, “Inquiry into the Variolae vaccinae Known as the Cow Pox”, in which he described the protective effect of cowpox against smallpox. Following Jenner’s work, the second generation of vaccines was introduced in the 1880s by Louis Pasteur, who developed vaccines for chicken cholera and anthrax. Vaccines then became a matter of national prestige in the late nineteenth century. National vaccination policies were adopted and compulsory vaccination laws were passed. Vaccinology flourished in the twentieth century. There was an emergence of several successful vaccines, including those against diphtheria, measles, mumps, and rubella (MMR). Major achievements included the development of the polio vaccine in the 1950s and the eradication of smallpox during the 1960s and 1970s. In the early 1950s, four vaccines were available: diphtheria, tetanus, pertussis and smallpox. Maurice Hilleman was the most prolific of the developers of the vaccines in the twentieth century He was responsible for more than 40 vaccines, including: MMR, pneumonia, and meningitis. As vaccines became more common and the major diseases they prevented seemed to be eradicated., many people began taking them for granted. Today, there is controversy about whether or not to be vaccinated in many cases. However, vaccines remain elusive for many important diseases, including herpes simplex, malaria, gonorrhea, and HIV.
(Sources: Centers for Disease Control and The Children’s Hospital of Philadelphia)
How preventive vaccines work
In the case of diseases caused by viruses (e.g., measles, polio, and smallpox) and bacteria (e.g., diphtheria, tetanus, and tuberculosis), vaccines work by exposing people to a weakened or inactivated version of the threat. This enables their immune system to find these threats according to their specific markers—known as “antigens”—and mount a response against them. These vaccines typically work best in the preventive setting when an individual is given the vaccine before being infected by the bacteria or virus. In order to understand how a vaccine functions, we need to understand the basics of immune system and how the immune response works by explaining the body’s natural response.
A pathogen is a bacterium, virus, parasite, or fungus that causes a disease within the body. Every pathogen is composed of many subparts, usually unique to the specific pathogen and the disease it causes. That specific subpart of a pathogen that causes the formation of antibodies is called an antigen. The antibodies produced in response to the pathogen’s antigen are an important part of the immune system. Consider antibodies as the key defense force in the body’s system. Each antibody is trained to recognize one specific antigen. There are thousands of different antibodies in our bodies. When the human body is exposed to an antigen for the first time, it takes time for the immune system to respond and produce antibodies specific to that antigen. In the meantime, the person is susceptible to becoming ill. Once the antigen-specific antibodies are produced, they work with the rest of the immune system to destroy the pathogen and stop the disease. The body then produces antibodies in its primary response to an antigen and creates memory cells to remember the specific pathogen and prompt the immune response to destroy those foreign cells if infected with the same pathogen in the future. The immune system will be able to respond immediately, and provide protection against diseases.
Vaccines contain weakened or inactive parts of antigens that trigger an immune response within the body. Newer vaccines have the blueprint for producing antigens rather than having the antigen itself. Regardless of whether the vaccine is made up of the antigen itself or its blueprint, this weakened version will not cause the disease in the person receiving the vaccine, but it will prompt their immune system to respond much as it would have on its first reaction to the actual pathogen. Some vaccines require multiple doses, given weeks or months apart. This is sometimes needed to allow to produce long-lived antibodies and the development of memory cells. In this way, the body is trained.
Certain factors determine the need of vaccines, which together are known as “HALO’’.
- Health – some people may benefit from additional or more frequent immunizations due to health factors; such as, pregnant women, premature babies, or those with conditions such as asthma, diabetes, HIV and disorders of the heart, lungs, spleen or kidneys.
- Age – at certain ages, we are more vulnerable to some illnesses; such as, in childhood, in secondary school and when we are older.
- Lifestyle – some lifestyle choices can put us or the community at risk; such as, overseas travel, becoming a new parent, sexual activity, smoking, or playing contact sports.
- Occupation – some jobs have a higher risk of exposure to infections; such as, those who work in healthcare, childcare and emergency services.
(Sources: World Health Organization)
What do preventive vaccines contain
Depending on the infection, ingredients in vaccines can vary. They may also change from year to year as new strains of viruses (such as the flu) appear. Some vaccines may contain a small dose of:
- a live (but weakened) germ
- dead germs
- small parts of germs (for example, a molecule from the surface of a germ)
- inactivated toxins produced by bacteria
- antibiotics or preservatives to stop the vaccine from becoming contaminated or expiring
- diluents (such as sterile water or saline).
Live, attenuated vaccines: live, attenuated vaccines are the closest to a natural infection. They contain a weakened version of a living virus or bacteria. These types of vaccines teach your immune system what the infection might look like without causing a severe illness. But because these vaccines contain living pathogens, they can’t be given to people with weak immune systems. The MMR and chickenpox vaccines are examples of live, attenuated vaccines.
Inactivated vaccines: Inactivated vaccines contain an inactivated or dead version of a virus or pathogen. They are not as much like a live infection, so often people need multiple doses of this kind of vaccine to maintain immunity. These are safer for people who are immunocompromised. The injectable flu vaccine is an inactivated vaccine, as is the polio vaccine currently distributed in the United States.
Subunit: vaccines contain only parts of a virus or bacteria instead of a whole pathogen.
This lets your immune system directly target the important antigen of the pathogen and tends to have fewer side effects than inactivated or live attenuated vaccines. The whooping cough, or pertussis, component of the TDaP vaccine is a subunit vaccine.
There are other kinds of vaccines, that are specialized to deal with unique types of bacteria and bacterial toxins, like conjugate and toxoid vaccines. For example, the TDaP vaccine contains diphtheria and tetanus toxoids.
Some new kinds of vaccines are being developed, including mRNA and vector-based vaccines. These use your cell’s own machinery to produce antigens for certain pathogens. These new types of vaccines may lead to safer and easier-to-produce vaccines against diseases in the future.
(Sources: Centers for Disease Control, The University of Chicago Medical Centerand Better Health Channel)
Route of administration
Oral route: is administered through drops to the mouth. Rotavirus vaccine (RV1 [Rotarix], RV5 [RotaTeq]) is the only routinely recommended vaccine administered orally. Rotavirus vaccine should never be injected.
Intranasal route: is administered into each nostril using a manufacturer-filled nasal sprayer. Live, attenuated influenza (LAIV [FluMist]) vaccine is the only vaccine administered by the intranasal route.
Subcutaneous route: is administered into the fatty tissue found below the dermis and above muscle tissue.
Intramuscular route: is administered into the muscle through the skin and subcutaneous tissue.
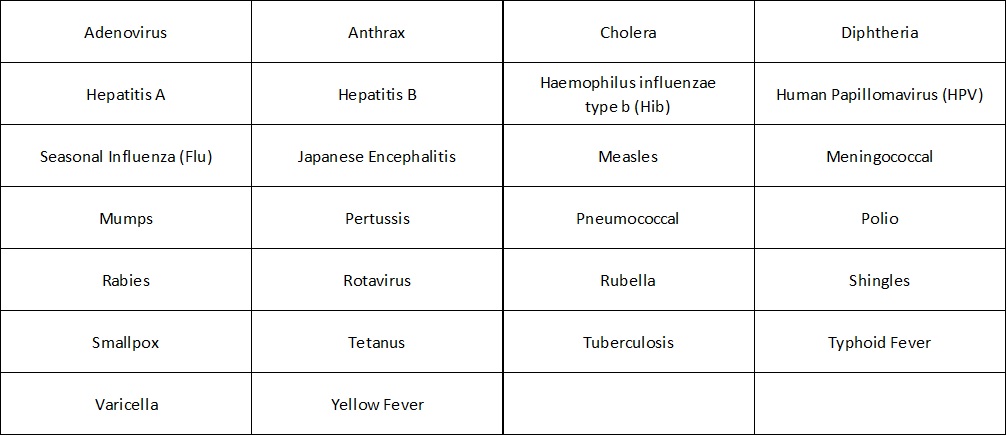
Here are the recommended vaccinations for given diseases with their respective vaccine names.
(Sources: Centers for Disease Control)
Preventive cancer vaccines
In the case of cancer, the situation is more complicated for several reasons, leading to increased difficulty in developing vaccines to either prevent or treat cancer. Unlike bacteria and viruses, which appear foreign to our immune system, cancer cells more closely resemble our normal, healthy cells. Furthermore, everyone’s tumor is in some sense unique and has its own distinguishing antigens. As a result, more sophisticated approaches are necessary to develop effective cancer vaccines.
These are preventive vaccines that target the viruses which cause certain cancers. They may help protect against some cancers, but they don’t target cancer cells directly because cancer cells have not yet been formed or found. These types of vaccines are only useful for cancers known to be caused by infections, but most cancers, including colorectal, lung, prostate, and breast cancers, are not thought to be caused by infections.
These vaccines are:
Cervarix®: a vaccine approved for use in preventing infection by the two strains of HPV that cause most cervical cancers, HPV types 16 and 18; can help prevent the development of HPV-related anal, cervical, head and neck, penile, vulvar, and vaginal cancers.
Gardasil®: a vaccine that protects against infection by HPV types 16, 18, 6, and 11; can help prevent the development of HPV-related anal, cervical, head and neck, penile, vulvar, and vaginal cancers.
Gardasil-9®: a vaccine approved for the prevention of infection by HPV types 16, 18, 31, 33, 45, 52, and 58, and for the prevention of genital warts caused by HPV types 6 or 11; can help prevent the development of HPV-related anal, cervical, head and neck, penile, throat, vulvar, and vaginal cancers.
Hepatitis B (HBV) vaccine (HEPLISAV-B®): a vaccine that protects against infection by the hepatitis B virus and prevents liver cancer.
(Sources: National Cancer Institutes of Health and U.S. Food & Drug Administration )
Future of preventive vaccines
Advances in vaccine technology are crucial to limit and prevent infectious diseases around the world, which still account for around 40% of all recorded deaths globally. Changing how existing vaccines are used, developing new vaccine delivery technologies and generating new vaccines are some of the ways researchers are working to overcome this ongoing challenge and save lives. Many technologies under development will improve the effectiveness of vaccine delivery and make it simpler. To make a vaccine that only needs to be given once, it must either be very powerful or packaged so that its contents are released intermittently once it has been administered. Technologies and alternative adjuvants that can remove the need for multiple shots are under development.
Currently, many vaccines need to be injected—an experience that people can find unpleasant and may be a serious psychological barrier for some. Needle-free administration is already possible for some vaccines, such as live vaccines given orally (e.g. rotavirus). Researchers are working on edible plant-based vaccine materials, needle-free skin patches and microneedle injection technologies to get the vaccine through the skin without discomfort. Technologies for delivering multiple antigens in one injection are improving. Many different inactivated vaccines can already be given in one injection without impairing the immune response and some live virus vaccines can also be given in one injection. That means fewer needles for patients and more efficient vaccine delivery overall. In terms of prevention of infectious diseases, disinfection can be applied to reduce the risk of transmission of pathogens from patient to patient and health-care workers to patients.